For decades, healthcare professionals have trusted products from DonJoy®, Chattanooga®, and Aircast® to deliver exceptional patient outcomes. These iconic brands, part of the Enovis™ family, have shaped orthopedic care and rehabilitation across the globe. Today, Enovis—a worldwide leader in medical technology solutions—announces a strategic visual transformation that unites these trusted names under a cohesive brand identity while preserving their individual legacies of innovation.
The Enovis Family: A Legacy of Innovative Brands
Enovis encompasses approximately a dozen specialized product brands within its comprehensive portfolio. Each brand brings distinctive expertise to the continuum of care, from prevention and rehabilitation to surgical intervention. Let’s explore the remarkable journeys of three cornerstone brands:
DonJoy® – Protecting Knees (and More) Since the 1970s
DonJoy has become virtually synonymous with knee bracing excellence. This cornerstone Enovis brand has manufactured and supplied braces for knee ligament protection since the late 1970s, utilizing patented technology specifically designed to reduce anterior cruciate ligament (ACL) strain1,2.
The Garage That Changed Orthopedics
In 1978, Philadelphia Eagles’ offensive line captain Mark Nordquist and lawyer Ken Reed founded a small company in a Carlsbad, California garage. They named their venture DonJoy after their wives, Donna and Joy—a personal touch that reflected their commitment to improving patients’ lives.
DonJoy initially focused on developing knee braces, and by the late 1990s, it was generating approximately $100 million in annual revenues through an expanding range of orthopedic products. Following a series of strategic acquisitions and mergers, the company evolved into DJO and later, Enovis. Throughout these transformations, the DonJoy name has endured for almost half a century, proudly displayed on products worn by millions worldwide.
Flagship Product: Defiance® PRO
The Defiance® PRO represents the culmination of decades of research in knee stability engineering. This custom-fit functional knee brace features aircraft-grade aluminum and proprietary hinge technology that mirrors natural knee movement while providing crucial support for ACL, PCL, MCL, and LCL injuries. Professional athletes and weekend warriors alike rely on its lightweight yet robust design for confidence during activity.
Aircast® – Over Half a Century in Service of Medical Professionals
For more than 50 years, medical professionals worldwide have depended on Aircast for technological breakthroughs in patient care.
Rooted in sound scientific methods, each Aircast product is developed using the concept of “functional management,” setting progressive standards of care for lower limb fractures, ankle sprains, and other injuries with patented technology and graduated pneumatic compression.
Aircast was founded in 1972 by U.S. inventor Glenn Johnson Jr. after he created the eponymous pneumatic ankle brace system. The innovative air cell technology provides targeted compression and stabilization while allowing appropriate movement—a revolutionary approach to ankle injury management. Among Johnson’s other inventions was the VenaFlow™ system, a DVT-prevention device used in hospitals worldwide.
Flagship Product: AirSelect™ Walker
The AirSelect™ Walker exemplifies Aircast’s commitment to functional recovery. Its SoftStrike technology absorbs shock and reduces heel loading, while integrated air cells deliver customized compression. The intuitive pump system allows patients to adjust pressure levels independently, promoting compliance and improving outcomes. Clinical studies have demonstrated faster recovery times compared to traditional immobilization methods for appropriate indications.3,4
Chattanooga® – Supporting Physiotherapists Since 1947
Founded in Chattanooga, Tennessee, by local athletic trainer Lee Jensen and his business partner Jack Walker, the Chattanooga Group began as Chattanooga Pharmacal Company in 1947.
From Local Startup to Global Leader
The company initially created hot and cold therapy products for the physiotherapy market before expanding its innovation focus. A significant breakthrough came with the development of the Intelect line, which brought portable ultrasound and electrotherapy devices into private clinics and transformed treatment accessibility.
By the early 2000s, Chattanooga had established itself as the world’s largest manufacturer of rehabilitation equipment, contributing to improved treatment outcomes in hospitals, clinics, and home settings worldwide. After nearly 80 years, the Chattanooga brand continues to be associated with technological advancements in treating musculoskeletal, neurological, and soft tissue disorders.
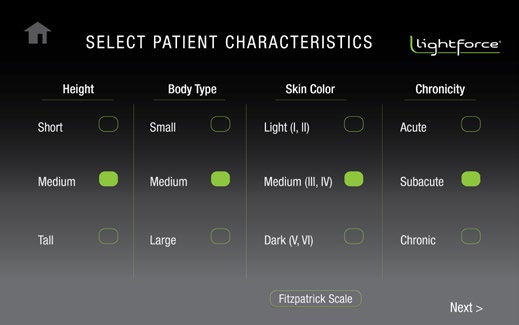
Flagship Product: LightForce® Laser
The LightForce® laser therapy system represents a significant advancement in non-invasive pain management. Using specific wavelengths of light to penetrate tissue and stimulate cellular metabolism, this photobiomodulation therapy helps reduce inflammation and relieve pain.5 Clinicians appreciate its intuitive interface and customizable treatment protocols that address a wide range of conditions from tendinopathies to post-surgical recovery.
Introducing the Updated Enovis Product Brands
As a family of brands under the banner of Enovis, DonJoy, Aircast, Chattanooga, and their sister brands now share a cohesive visual identity that clearly communicates their relationship while honoring their individual histories.
The refreshed type treatment applied to the product brand logos achieves a unified aesthetic while creating a clear hierarchy between the corporate brand and its product brands. The updated design maintains recognizable elements from each brand’s heritage while bringing them into alignment with Enovis’s forward-looking vision.
For healthcare professionals who have relied on these trusted brands throughout their careers, this unified identity signals not an ending but a strengthening—a commitment to continued excellence and innovation under the Enovis banner for decades to come.
Healthcare professionals interested in learning more about Enovis products can contact their local Enovis representative.
References
- Fleming BC et al. The influence of functional knee bracing on the anterior cruciate ligament strain biomechanics in weightbearing and nonweightbearing knees. Am J Sports Med 2000;28(6):815-24.
- Lin CF, Liu H, Garrett WE, Yu B. Effects of a knee extension constraint brace on selected lower extremity motion patterns during a stop-jump task. J Appl Biomech. 2008 May;24(2):158-65.
- Shahid MK, Punwar S, Boulind C, Bannister G. Aircast walking boot and below-knee walking cast for avulsion fractures of the base of the fifth metatarsal: a comparative cohort study. Foot Ankle Int. 2013 Jan;34(1):75-9.
- Haworth L, Booth N, Chohan A, Chapman G, Richards J. How does orthotic walker boot design influence lower limb and trunk function during gait? Prosthet Orthot Int. 2024 Mar. E-Pub ahead of publication.
- Chatterjee P, Srivastava AK, Kumar DA, Chakrawarty A, Khan MA, Ambashtha AK, Kumar V, De Taboada L, Dey AB. Effect of deep tissue laser therapy treatment on peripheral neuropathic pain in older adults with type 2 diabetes: a pilot randomized clinical trial. BMC Geriatr. 2019 Aug 12;19(1):218.